Addressing Diabetes Care
The American Diabetes Association (ADA) is embarking on an Overcoming Therapeutic Inertia (OTI) initiative to address all the forces and factors that contribute to delays in implementing the most effective care for each person with diabetes.
“Therapeutic inertia” is a lack of timely adjustment to therapy when a patient’s treatment goals are not met. In diabetes care, it means being slow to add or change the care plan if a patient’s A1C is too high. The care plan may include medications, health checks, diabetes education, nutrition therapy, exercise, and emotional support.
Consider downloading our plain-language fact sheet and sharing it with your staff and colleagues: Getting to Goal: Overcoming Therapeutic Inertia in Diabetes Care.
The Pillars of Overcoming Therapeutic Inertia
Taking Aim With
the OTI Initiative
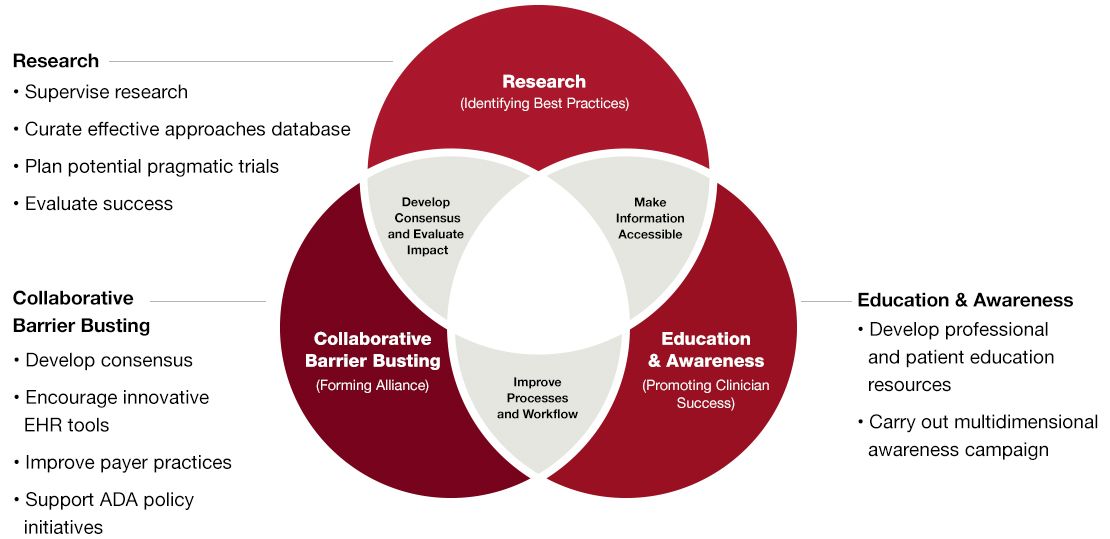
The OTI initiative was conceived to develop practical, real-world solutions to this complex problem that is adversely affecting outcomes for people living with type 2 diabetes. Its overall goal is to promote the adoption of evidence-based practices, strategies, programs, and tools that address key barriers in diabetes care, leading to more timely treatment modification and improved outcomes.
Our priorities are rooted in research, education, and collaborative barrier busting.
What Can I Do Now?
Overcoming this problem requires ongoing effort, but there are some steps you can take right away.
Common Questions
- What is diabetes therapeutic inertia?
-
“Therapeutic inertia” is a lack of timely adjustment to therapy when a patient’s treatment goals are not met. In diabetes care, it means being slow to add or change the care plan if a patient’s A1C is too high. The care plan may include medications, health checks, diabetes education, nutrition therapy, exercise, and emotional support.
- How common is therapeutic inertia in diabetes care?
-
The ADA recommends an A1C target of less than 7% for most people with diabetes. This goal can be set higher or lower based on each patient’s needs. However, fewer than two-thirds of people with type 2 diabetes get to their A1C goal, and only about half get to an A1C of less than 7%. Despite a wealth of new medicines, treatment tools, and best-practice guidelines, this number actually dropped over the past 10 years, while the number of patients with an A1C of more than 9% went up.
Delays happen at all stages of diabetes treatment, from starting the first drug to adding more medications or intensifying insulin therapy. The ADA advises clinicians to advance therapy if a patient doesn’t get to goal within 3 to 6 months. However, studies have shown that it often takes more than a year—and can take more than 7 years—to intensify a patient’s treatment. Likewise, elderly patients often remain in danger from overtreatment for too long. - Why is timely therapy adjustment so important?
-
Research has shown that managing glucose levels early on leads to better long-term outcomes and reduces a person’s chances of having a heart attack or stroke or developing other complications such as eye disease, kidney disease, and nerve damage. People who reach their A1C targets soon after finding out they have diabetes are more likely to keep their glucose in their target ranges. However, not reaching targets early reduces a person’s chances of doing so later in their treatment. It also deprives patients of a known “legacy effect,” through which good glucose management early on keeps reducing health risks many years later—even if a patient’s A1C eventually creeps up.
Here are some more alarming facts about the current diabetes landscape:- In the past 20 years, despite more technology, more education, and more drug therapies, the average A1C for a person with diabetes has not changed. The number of patients with an A1C over 9% has actually increased.
- Treatment intensification is significantly behind recommendations in the ADA Standards of Care.
- Only 5% of recently diagnosed patients with diabetes on Medicare are using diabetes self-management education and support (DSMES).
- Based on recent studies, there is a significant gap in what patients say they are willing to do to reduce A1C and what physicians believe patients are willing to do to reduce A1C.
- Real-time patient data indicate that within 1 year of a diabetes diagnosis, less than 50% of patients are still taking the prescribed medication.
- $327 billion was spent on treatment of people with diagnosed diabetes in 2017.
- What else should I know about this issue?
-
Diabetes education and nutrition therapy are key to helping patients share in their care planning and get to their clinical goals quickly. However, far too few people with type 2 diabetes get these services. To reap better outcomes, patients must be engaged in their own care and able to carry out daily diabetes self-management.
Hastening the pace of diabetes treatment also requires a team effort from all types of diabetes care providers and from the systems in which they practice. Advocacy groups, policymakers, insurance companies, and the drug and medical technology industries also have roles to play by improving patients’ access to the best possible diabetes care. - How can I tell if therapeutic inertia is a problem in my practice?
- 1. Assess your entire patient population
As a starting place, use your electronic health record (EHR) and look at all patients with type 2 diabetes. Many EHRs have an embedded diabetes registry. If you have one, use it. Check the following:
- How many have an A1C of 9% or higher with no recent visit or therapy change?
- How many have an A1C of 7%-8.9% with no recent visit or therapy change?
- How many have never had diabetes education or nutrition therapy?
- How many have not had an A1C in 12 months or more?
The answers to these questions will show how much therapy delays are keeping your patients from reaping the benefits of hitting their health goals early. Regularly repeating this process will show you if things are improving.
2. Engage with patients in real time
Check with patients one on one during visits for signs that their care is not advancing quickly enough. The box below shows a math formula that can be used to gauge how much a patient’s care is affected by therapeutic inertia. Such scores aren’t always very helpful in real-world practice, though. You can gain more insight simply by reviewing patients’ blood glucose log, A1C, and medications and then talking with them about any problems they may be having, such as cost concerns or worries about side effects. Together, you can then develop plans for reaching their treatment targets as quickly as possible.
Thoughts from
LeadershipIn view of most of the evidence being published in the area of failure of therapeutic goal achievement, we will restrict the initiative to the area of “failure to initiate, intensify, or de-intensify therapy when appropriate to do so.” In this initiative, we will consider all contributors to therapeutic inertia, including those at the health care professional, patient, and health system levels.
Kamlesh Khunti, MD, PhDCo-Chair, Overcoming Therapeutic
Inertia Steering Committee
Summing It All Up
The OTI initiative will serve as a catalyst for meaningful change throughout the diabetes “continuum of care.” Our goal is to either accelerate the pace at which clinicians advance diabetes therapy or improve the adoption and maintenance of therapeutic regimens. We aim to increase the number of people achieving and maintaining an A1C of less than 7% and decrease the percentage of those with an A1C more than 9%, while also reducing other diabetes complications.
Ultimately, we want to reduce the incidence of chronic diabetes complications and mortality, lower associated personal and societal costs, and improve long-term outcomes.
Alliance Partners for Overcoming Therapeutic Inertia
Alliance Partners are committed collaborating with the American Diabetes Association in various ways to support activities of the Overcoming Therapeutic Inertia initiative and to disseminate evidence-based findings and best-practice recommendations developed through the initiative.









