THERAPEUTIC INERTIA
Practice
Improvement
Resources
Overcoming Therapeutic Inertia in Type 2 Diabetes: Benefiting Patients, Clinicians, and Health Systems
Build awareness of the problem of therapeutic inertia in people with type 2 diabetes and advocate for changes to overcome it. Download this presentation to help decision-makers in your organization understand that improved health outcomes and efficiencies can be achieved by overcoming therapeutic inertia.
Download the presentation now!
An Implementation Guide to Overcoming Therapeutic Inertia in Diabetes
Are the influencers and decision-makers in your organization aware of the problem of therapeutic inertia and ready to do something about it? Use this presentation to explore best practices and strategies to help overcome therapeutic inertia in your organization.
Download the presentation now!
Using EHRs to Help People Living with Type 2 Diabetes Achieve Their A1C Targets
Our new practice guide will help you leverage your electronic health records to identify and intervene in the care of adults living with type 2 diabetes who may be experiencing therapeutic inertia. Watch our how-to video and download the guide.
Explore the guideDownload Infographics
Identify the right patient at the right time for insulin treatment and use these infographics to help you and other diabetes care team members initiate, intensify, and de-intensify insulin at the right time.Leveraging the Best Practices Framework
Our evidence- and consensus-based recommendations leverage insights and real practice experiences from our work group members.
These action-based recommendations are at the core of our educational and awareness activities. We are in the process of building educational programming, action guides, and point-of-care tools to help primary care clinicians and practices integrate these recommendations into practice.
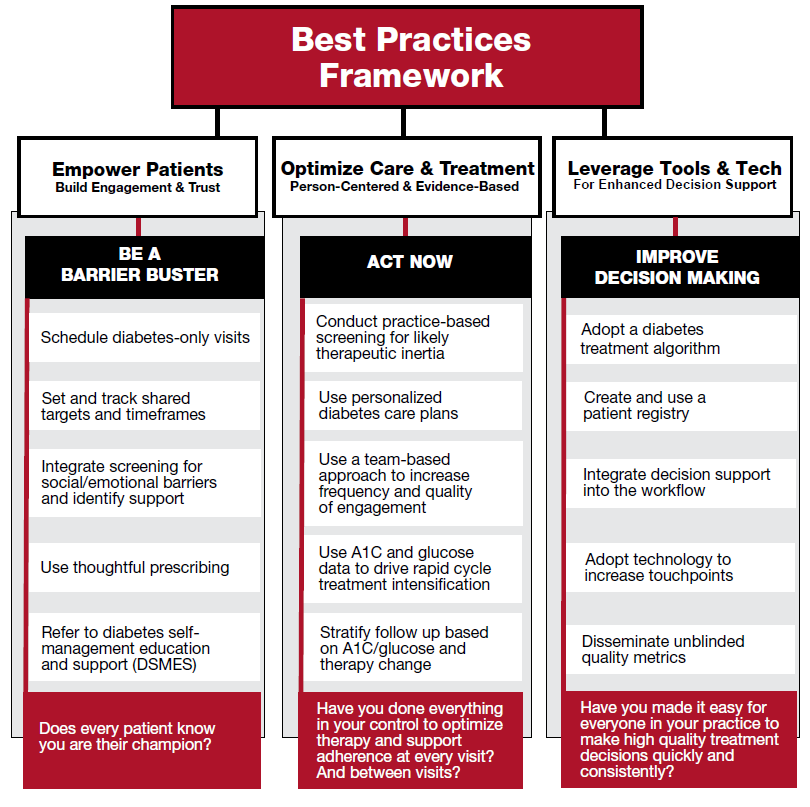
- Empower Patients | Build Engagement & Trust
-
- Schedule diabetes-only visits:
All too often, urgent and emergent challenges take precedence during office visits. By prioritizing diabetes at least once a year, you have the opportunity to really focus on setting shared goals, developing a diabetes care plan, assessing barriers, evaluating gaps in current diabetes knowledge, and building rapport and trust. These appointments will also serve to deliver the message about the importance of managing diabetes to your patients. - Set and track shared targets and timeframes:
The heart of overcoming therapeutic inertia (OTI) is setting realistic and personalized goals with full buy-in from the person with diabetes. With strong evidence for the positive legacy impact of achieving normal or near-normal glucose early, having a clear timeframe for reaching these goals is just as important as a realistic therapy intensification strategy. - Integrate screening for social or emotional barriers and identify support:
While timely therapy intensification is essential for OTI, evidence shows it is not sufficient. Identifying barriers to a patient’s care plan follow-through is critical. Barriers can include financial challenges, food and housing insecurity, transportation issues, diabetes distress, depression, and low health literacy. Once barriers are identified, locate support services in your community and make referrals. Consider ways to leverage existing staff to help with this task. - Use thoughtful prescribing:
Before making therapy recommendations, be sure to understand personal preference, concerns about cost, and fears that may drive poor medication-taking behavior. By asking and listening, you are building trust and high-quality engagement. You can use what you discover to collaborate with the patient. Through shared decision-making, you can improve follow-through and get to the patient’s goal faster. - Refer to diabetes self-management education and support (DSMES) services:
Although DSMES has been shown to improve health outcomes for people with diabetes, it is still greatly underutilized. By discussing the benefits of DSMES, consistently making referrals, and following up, you can increase the likelihood that people with diabetes will eventually take advantage of DSMES. Various forms of effective DSMES are now available and reimbursable, including web-based delivery. Find a program near you.
- Schedule diabetes-only visits:
- Optimize Care & Treatments | Person-Centered & Evidence-Based
-
- Conduct practice-based screening for likely therapeutic inertia:
Therapeutic inertia often goes undetected in the clinical practice. Having a clear process in place to identify and flag people with diabetes who are staying above target and not achieving goals in a timely manner can ensure that nobody is overlooked in a busy office setting. For example, use your electronic health records’ (EHR) registry feature to identify patients with an A1C equal to or greater than 9% who have not had a visit in the past 3 to 6 months—it is likely most of this cohort is experiencing therapeutic inertia. - Use personalized diabetes care plans:
Create and share a diabetes plan for every person with diabetes in your practice. Include glucose targets and timeframes to reach targets. Use a shared decision-making approach considering personal preferences, values, strengths, and medical, social, and psychological needs when developing or updating the care plan. - Use A1C and glucose data to drive rapid-cycle treatment intensification:
Using all available glucose data to drive therapy intensification is crucial to overcoming therapeutic inertia. If you rely solely on an A1C taken every 3 to 6 months to inform therapy adjustment, you may have people with diabetes above goal for long periods of time. Leveraging point-of-care A1C testing, continuous glucose monitors (CGM), and/or self-monitoring of blood glucose (SMBG) data improves point-of-care decision-making and supports rapid-cycle therapy intensification approaches. - Stratify follow-up based on A1C/glucose and therapy change:
Arrange more frequent visits based on A1C or glucose data and any recent therapy changes. Leverage telehealth to make this process easier for patients. For example, every 6 to 8 weeks for those at 9% or higher, every 2 to 3 months for those between 7% and 8.9%, and every 3 to 6 months for those less than 7% or at their personal target.
- Conduct practice-based screening for likely therapeutic inertia:
- Leverage Tools & Tech | For Enhanced Decision Support
-
- Adopt a diabetes treatment algorithm (simple and unambiguous):
Work with your entire care team to agree on and adopt a diabetes treatment algorithm that everyone uses. We recommend the American Diabetes Association’s (ADA’s) algorithm, of course, but the most important thing is consistency. Some offices find that making print copies, laminating them, and placing copies in each exam room is helpful. Many clinicians have also found ADA’s Standards of Care app to be a greattool to support better point-of-care decision-making. - Create and use a patient registry:
Patient registries, embedded in many EHRs, can be a valuable tool in addressing therapeutic inertia. Your medical practice or health systems can extract and summarize clinical data, such as diagnosis codes, lab tests, and medication records, from individual patient records to measure overall care quality. This data can then be used to identify patients going long periods above target who need additional engagement and support to reach their goal. - Integrate decision support into the workflow:
Use an EHR-based decision support tool, ADA’s Standards of Care app, or even a paper-based algorithm to improve decision quality and reduce decision fatigue. Beyond treatment-related decisions, these tools can also support the consistent assessment of patient-level barriers to care, like housing or food insecurity, depression, and financial challenges. Anything easily integrated into the workflow is better than nothing. - Adopt technology to increase touch points:
When it comes to engagement, both quantity and quality matter. Frequent touch points are important for optimizing disease management, building trust, and monitoring progress. Consider arranging more frequent office visits, telehealth visits, use of texting, continuous glucose monitors (CGM), and leveraging a patient portal. - Disseminate unblinded quality metrics:
Identify positive outliers. By identifying clinician approaches and practices that are achieving the best results and sharing this information, you support a learning culture that drives continuous quality improvement. Transparency, mutual support, and open communication among staff are essential for overcoming therapeutic inertia.
- Adopt a diabetes treatment algorithm (simple and unambiguous):
Explore Pro and Practice Pearl Videos
Care professionals can get the diabetes support they need to provide faster care and fight therapeutic inertia with informative videos. Explore resources now!Clinical Self-Assessment Tools

Therapeutic Inertia in Clinical Practice:
Self-Assessment
Use this tool to measure how often therapeutic inertia occurs in your practice and to identify contributing factors. This tool can also be used to help detect therapeutic inertia between visits.
Take the Survey
Clinical Self-Assessment Tool
Helping people living with diabetes get access to timely, effective care is a goal all care providers have. Take our assessment test and learn how be an inertia buster and give patients an optimal health care experience.
Download Now